Your going to find this same basic advice on pretty much every site. This is pretty well the standard approach, but we felt like we would not be complete if we didn’t include it here.
On exam day, you will be standing in front of the examination room door. The timer will start, you’ll pull back the flap hiding the patient info, and away you go. The following should take about 30 seconds or less.
- Write down the patient’s name, demographic info, chief complaint and vital signs at the top of the paper. Vital signs is maybe a little debatable. Some people would say to only write down the ones that are abnormal. I see their point, but these are numbers that I want to be able to reflect on regularly. Depending on the patient, seemingly normal vital signs turn out to be very abnormal. Ever treat someone with hypertension who usually has a systolic in the 140s and all of the sudden today, they’re dizzy with a systolic in the 110s?
- Make a giant cross on your paper, like this. (We’ll probably put a printout sample in the cheat sheet section of the website)
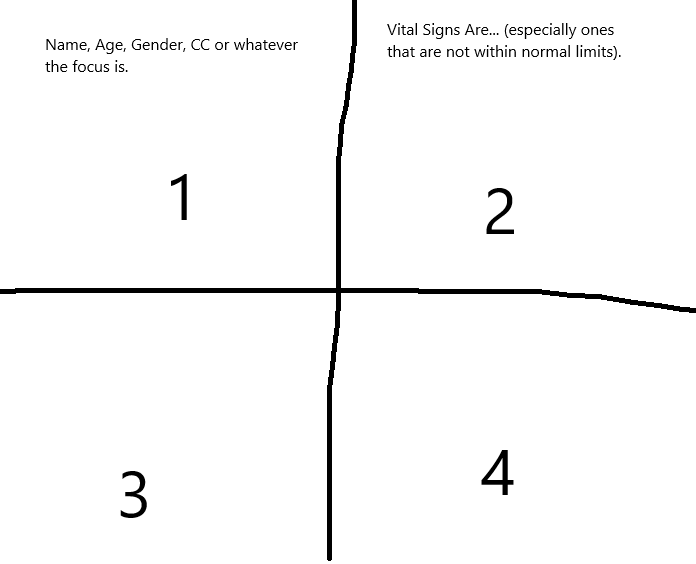
- Start with section 4. Write down a preliminary ddx and the templated exams that you will probably want to do. So, if someone has a chief complaint of chest pain, I’d probably right down “cardiac” (because there are a ton of them), “pulmonary – asthma” and “GERD.” Not very precise, but they have me thinking across the body systems that could be involved. Then, I’m going to write down CVS, pulm and abd since those are the exams I’m going to want to be sure to cover. The goal here is that even before walking in, I have already automated as much as this as possible.
Section 1 gets the HPI, section 2 gets ROS and 3 gets all the extra past history that you want to add in. You may want to write in the mnemonic before you go in, which would take extra time. Or you may want to write the mnemonic as you ask the questions during the interview, which might leave you with a blank moment and stuttering about what to say next.
You may decide to make some changes to this, which is totally cool. This method or some variation is what the vast majority of students use. That being said, absolutely tweak the hell out of it to make sense to you. You’re the one using it, after all!
Let’s take a brief look at the mnemonics I used and then wrap this up.
Section 1 is where you start your HPI:
L – location
I – intensity (scale 1-10)
Q – quality
O – onset
R – radiation
P – progression
D – duration
F – frequency
C – chronic vs acute (have you had this before?)
S – setting
A – alleviating factors
A – aggravating factors
A – associated symptoms
Section 2 is ROS. I write the mnemonic out, and then mostly just put a check mark for when there is a positive response. Occasionally, I’ll add a note to it if it is pertinent. For the exam, focus on the things that are important and skip what you don’t really need:
T – trauma
H – headache
E – edema (swelling)
N – nausea and/or vomiting
F – fever
R – rash, racing heart (I hate it when one letter stands for multiple).
C – cough, chest pain, cold symptoms (even worse)
S – shortness of breath
P – pain in joints
U – urination
B – bowels
S – sleep
A – appetite
W – weight
I – infections (recent ones) and recent infectious contacts
D – depression/mood
Section 3 is all the other history things that didn’t get covered:
P – past medical history
A – allergies
M – medicines
H – hospitalizations
I – immunizations
T – travel
S – surgeries
F – family history
O – occupation
O – ob/gyn
S – sexual
S – social (alcohol, tobacco, drugs, diet and exercise)
These cover pretty much the majority of the bases every time. It does not cover specific questions you need to ask as they relate directly to the chief complaint. They also have some questions included that you don’t really need. The danger is to have these down well enough to use them but not so well that you’re unable to stray away from them. They’re a crutch at first, just make sure you can walk on your own at some point. For the exam, make sure to stay relevant to the chief complaint.
Last piece of advice, get started using these early! If you incorporate them to your process from the start of clinicals, you will have this down cold by the time that you get to the exam!
Keep studying!
